6.2 Seizures and epilepsy
From 22 June 2022 there have been changes to the fitness to drive criteria for seizures and epilepsy.
See Summary of changes for more details
In this section
6.2.1. Relevance to the driving task
6.2.2. General assessment and management guideline
6.2.3. Medical standards for licensing
Refer also to section 1. Blackouts and section 2. Cardiovascular conditions.
6.2.1 Relevance to the driving task
Effects of seizures on driving1, 2, 3
Seizures vary considerably, some being purely subjective experiences – for example, some focal seizures – but most involve some impairment of consciousness (e.g. absence and focal impaired awareness seizures) or loss of voluntary control of the limbs (e.g. focal motor and focal impaired awareness seizures). Convulsive (tonic–clonic) seizures may be generalised from onset or have a focal onset. Seizures associated with loss of awareness, even if brief or subtle, or loss of motor control, have the potential to impair the ability to control a motor vehicle.
Evidence of crash risk4, 5, 6
Most studies have reported an elevated crash risk among drivers with epilepsy, but the size of the risk varies considerably across the studies. These studies have found that people with epilepsy are twice as likely to be involved in a motor vehicle crash compared with the general driving population. More recent studies have found that drivers who do not take antiseizure medication as prescribed are at an increased risk for experiencing a crash.
6.2.2 General assessment and management guideline
Epilepsy refers to the tendency to experience recurrent seizures. Not all people who experience a seizure have epilepsy.
Epilepsy is a common disorder with a cumulative incidence of 2 per cent of the population, with 0.5 per cent affected and taking medication at any one time. Most cases respond well to treatment, with a terminal remission rate of 80 per cent or more. The majority suffer few seizures in a lifetime, and about half will have no further seizures in the first one or two years after starting treatment. Some people with epilepsy may eventually cease medication. For others, surgery may be beneficial.
In general, responsible people with well- managed epilepsy (as demonstrated by an appropriate seizure-free period and compliance with treatment and other recommendations) may be considered by the driver licensing authority to be fit to drive a private vehicle. Conditional licences rely on individual responsibility for management of the condition, including compliance with treatment, in conjunction with the support of a health professional and regular review.
Commercial vehicle driving exposes the driver and the public to a relatively greater risk because of the increased time spent at the wheel, as well as the generally greater potential for injury from motor vehicle crashes due to the greater size or weight of commercial vehicles, or large numbers of passengers carried. For this reason, the acceptable risk of a seizure-related crash for commercial driving is much less, and the requirements applied are much stricter; in addition, sleep deprivation is a common provoking factor in epilepsy and may be experienced in long-distance transport driving and amongst drivers doing shift work.
It is good medical practice for any person with initial seizures to be referred to a specialist, where available, for accurate diagnosis of the specific epilepsy syndrome so that appropriate treatment is instituted and all the risks associated with epilepsy, including driving, can be explained.
With regard to licensing, the treating doctor or general practitioner may liaise with the driver licensing authority about whether the criteria are met for driving a private vehicle, but only a specialist may do so for a commercial vehicle driver.
Use of electroencephalograms (EEG)9, 10
Electroencephalography is an important tool in diagnosing epilepsy. In people who have had one or more seizures, it has a limited but valuable role in predicting seizure recurrence. It may also be used to identify subtle episodes in which awareness may be impaired. Because there is a wide range of clinical situations, with varying utility of EEG, it does not form part of the driving standards except for the initial fitness assessment of commercial drivers. When epileptiform abnormalities that may represent subtle seizures (e.g. generalised spike-wave bursts lasting longer than three seconds, or photoparoxysmal response) are found on the EEG of those who meet the standard to hold a conditional (or unconditional) licence, their fitness should be assessed on a case-by-case basis. This may require more detailed testing.
Advice to licence holders
All licence holders should be advised of the following general principles for safety when driving:
- The person must continue to take antiseizure medication regularly as recommended.
- The person should ensure they get adequate sleep and not drive when sleep- deprived.
- The person should avoid circumstances, or the use of substances (e.g. excessive alcohol), that are known to increase the risk of seizures.
It is good medical practice for any person with epilepsy to be reviewed periodically. Patients who are licence holders should also be monitored regarding their response to treatment and compliance with the general advice for safety when driving. Drivers of private vehicles who hold a conditional licence should be reviewed at least annually by their treating doctor (unless experiencing an extended seizure-free period – see The default standard ). Commercial vehicle drivers should be reviewed at least annually by a specialist regarding any conditional licence that has been issued.
Refusal of medical advice
Some people with epilepsy choose not to follow medical advice, including the taking of antiseizure medicine and avoidance (where possible) of factors that may provoke seizures. If a patient refuses to follow a treating doctor’s recommendation, the patient should be assessed as not fit to drive. The treating doctor may consider reporting this information to the driver licensing authority so it can be considered in the event that another doctor certifies the person as fit to drive without therapy. Further guidance on managing patients who refuse to follow medical advice can be found in Part A section 3.3.1. Confidentiality, privacy and reporting to the driver licensing authority.
Refer also to Medication noncompliance and Uncertain or unreliable history in this section.
Concurrent conditions
Where epilepsy is associated with other impairments or conditions, the relevant sections covering those disorders should also be consulted.
Other conditions with risk of seizure
Seizures can occur in association with many brain disorders. Some of these disorders may also impair safe driving because of an associated neurological deficit. Both the occurrence of seizures, as well as the effect of any neurological deficit, must be taken into account when determining fitness to drive. Managing acute symptomatic seizures caused by a transient brain disorder or a metabolic disturbance (e.g. encephalitis, hyponatraemia, head injury or drug or alcohol withdrawal) is covered in the Neurological conditions . Refer also to section 6.3. Other neurological and neurodevelopmental conditions for seizures associated with a head injury and intracranial surgery.
Loss of consciousness due to other causes
In cases where it is not possible to be certain that loss of consciousness is due to a seizure or some other cause, refer to section 1.2.4. Blackouts of undetermined mechanism.
6.2.3 Medical standards for licensing
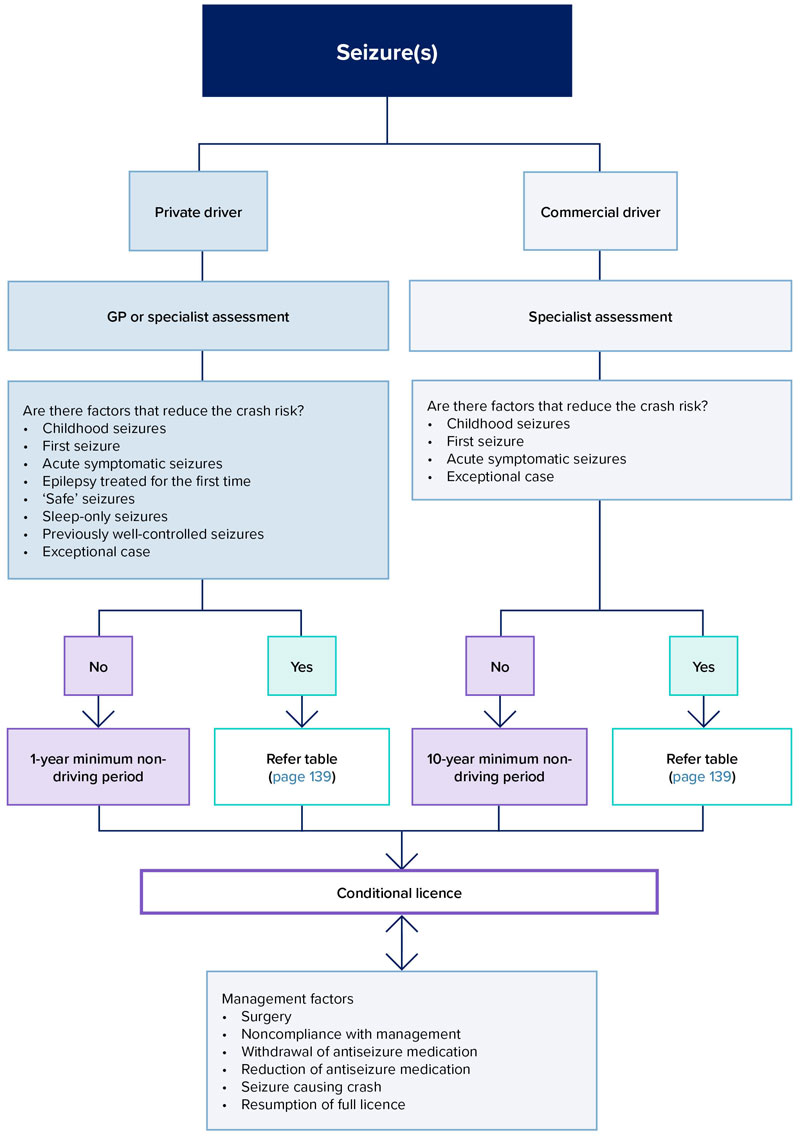
Given the considerable variation in seizures and their potential impact on safe driving, a hierarchy of standards has been developed that provides a logical and fair basis for decision making regarding licensing (see also Figure 13. Overview of management of a driver with seizures). This hierarchy comprises:
- a default standard, applicable to all cases of seizure, unless reductions are allowed (refer below and to the standards table)
- reductions for specific types of epilepsy or specific circumstances, including an allowance for exceptional circumstances upon the advice of a specialist in epilepsy (refer below and to the standards table).
In addition, advice is provided on a number of difficult management issues relating to safe driving for people with seizures and epilepsy (refer below and to the standards table).
The default standard (all cases)
The ‘default standard’ is the standard that applies to all drivers who have had a seizure unless their situation matches one of a number of defined situations listed in the table and described below. These situations are associated with a lower risk of a seizure-related crash and therefore driving may be resumed after a shorter period of seizure freedom than required under the default standard. However, the need to adhere to medical advice and at least annual review still apply. If a seizure has caused a crash within the preceding 12 months, the required period of seizure freedom may not be reduced below that required under the default standard. If antiseizure medication is to be withdrawn, the person should not drive (refer to table for details).
If a driver who is taking antiseizure medication has experienced an extended seizure-free period (more than 10 years for private drivers, and more than 20 years for commercial drivers) the driver licensing authority may consider reduced review requirements (at least once every three years) based on advice from the treating doctor or specialist.
Figure 13: Overview of management of a driver with seizures
Variations to the default standard
There are several situations in which a variation from the default standard may be considered by the driver licensing authority to allow an earlier return to driving. These are listed below and discussed on subsequent pages:
- seizures in childhood
- first seizure
- epilepsy treated for the first time
- acute symptomatic seizures
- ‘safe’ seizures
- seizures only in sleep
- seizures in a person previously well controlled
- exceptional circumstances.
In most cases, exceptions to the default standard will be considered only for private vehicle drivers. A reduction in restrictions for commercial vehicle drivers will generally only be granted after considering information provided by a specialist with expertise in epilepsy.
If a person has experienced a crash as a result of a seizure, the default non-driving seizure-free period applies, even if the situation matches one of those above.
In addition to the reduction for particular circumstances or seizure types, there is also an allowance for ‘exceptional cases’ in which a conditional licence may be considered for private or commercial vehicle drivers on the recommendation of a medical specialist with specific expertise in epilepsy. This enables individualisation of licensing for cases where the person does not meet the standard but may be safe to drive.
Licensing of drivers with a history of childhood febrile seizures or benign epilepsy syndrome of childhood
In some specific childhood epilepsy syndromes, seizures usually cease before the minimum age of driving. The driver may hold an unconditional licence if no seizures have occurred after the age of 11 years. If a seizure has occurred after 11 years of age, the default standard applies unless the situation matches one of those in this section (Variations to the default standard).
The first seizure (of any type)11,12, 13
The occurrence of a first seizure warrants medical specialist assessment, where available. Approximately half of all people experiencing their first seizure will never have another seizure, while half will have further seizures (i.e. epilepsy). The risk of recurrence falls with time. Driving may be resumed after sufficient time has passed without further seizures (with or without medication) to allow the risk to reach an acceptably low level (refer to the standards table). If a second seizure occurs (except on the same day as the first), the risk of recurrence is much higher. The standard for Epilepsy treated for the first time will then apply (refer to the standards table and to Figure 14).
Figure 14: Epilepsy treated for the first time
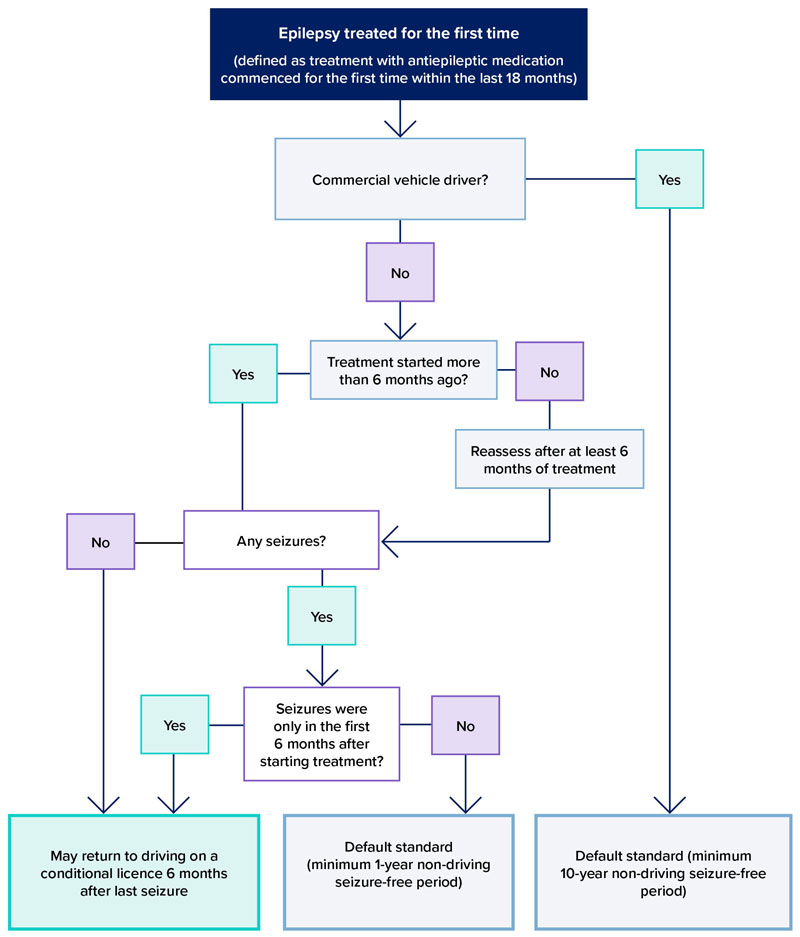
Epilepsy treated for the first time14,15
The risk of recurrent seizures in people starting treatment for epilepsy is sufficiently low to allow driving to resume earlier than required under the default standard. For the purpose of these standards, epilepsy treated for the first time means that treatment was started for the first time within the preceding 18 months.
When treatment with an antiseizure drug is started in a previously untreated person, enough time should pass to establish that the drug is effective before driving is recommenced. However, effectiveness cannot be established until the person reaches an appropriate dose. For example, if a drug is being gradually introduced over three weeks and a seizure occurs in the second week, it would be premature to declare the drug ineffective. The standard allows seizures to occur within the first six months after starting treatment without lengthening the required seizure-free period. However, if seizures occur more than six months after starting therapy, a longer seizure-free period is required (refer to table for details). For commercial drivers, the default standard applies.
For example, if a patient has a seizure three months after starting therapy, they may be fit to drive six months after the most recent seizure (nine months after starting therapy). However, if a person experiences a seizure eight months after starting therapy, the default standard applies and they may not be fit to drive until 12 months after the most recent seizure.
If the patient has received no treatment in the last five years or more, resumption of treatment is managed as if treated for the first time (as above).
Acute symptomatic seizures16,17
Acute symptomatic seizures are caused by a transient brain disorder or metabolic disturbance (e.g. encephalitis, hyponatraemia, head injury or drug or alcohol withdrawal) in patients without previous epilepsy. Acute symptomatic seizures can be followed by further seizures weeks, months or years after the transient brain disorder resolves. This may occur because of permanent changes to the brain caused by the process underlying the acute symptomatic seizures (e.g. seizures may return years after a resolved episode of encephalitis) or because the transient brain disorder has recurred (e.g. benzodiazepine withdrawal).
People who have experienced a seizure only during and because of a transient brain disorder or metabolic disturbance should not drive for a sufficient period to allow the risk of recurrence to fall to an acceptably low level (refer to table for details). Return to driving for commercial vehicle drivers requires input from an epilepsy specialist. The risk of seizure recurrence varies greatly, depending on the cause.
If seizures occur after the causative acute illness has resolved, whether or not due to a second transient brain disorder or metabolic disturbance, the acute symptomatic seizures standard no longer applies. For example, if a person has a seizure during an episode of encephalitis and then, after recovering from the encephalitis, has another seizure and begins treatment, the standard for epilepsy treated for the first time applies. Similarly, if a person experiences seizures during two separate episodes of benzodiazepine withdrawal, the default standard applies.
The management of late post-traumatic epilepsy is discussed in section 6.3.1. under Head injury.
‘Safe’ seizures (including prolonged aura)
Some seizures do not impair consciousness or the ability to control a motor vehicle; however, this must be well established without exceptions and corroborated by reliable witnesses or video- EEG recording because people may believe their consciousness is unimpaired when it is not. For example, some ‘auras’ are associated with impaired consciousness that the person does not perceive. Isolated infrequent myoclonic jerks (without impaired awareness) may be considered safe in the context of no seizures of any other type for more than 12 months.
For private vehicle drivers, where seizures occur only at a particular time of day (e.g. in the first hour after waking), a conditional licence, which limits driving to certain hours or circumstances, may be acceptable. This applies only to private vehicle drivers.
Seizures may begin with a subjective sensation (the ‘aura’) that precedes impairment of consciousness. If this lasts long enough, the driver may have time to stop the vehicle. However, this can only be relied upon when this pattern has been well established without exceptions and corroborated by witnesses or video-EEG monitoring. Furthermore, it may be impossible to stop immediately and safely because of traffic conditions. Even if the person is able to stop the vehicle before the seizure, they may then be in a confused state and not appreciate the danger of resuming their journey. For these reasons, such seizures can be considered safe only in exceptional circumstances and must be considered by the driver licensing authority on a case-by- case basis. See Exceptional cases in the text and table.
Any seizures that involve confusion/vagueness, automatisms, difficulty speaking or emotional features or memory loss are not considered safe seizures.
Sleep-only seizures
Some seizures occur only during sleep and hence are not a hazard to driving. In people who have never had a seizure while awake but who have an established pattern of seizures exclusively during sleep, the risk of subsequent seizures while awake is sufficiently low to allow private driving, despite continuing seizures while asleep. In people with an established pattern of sleep-only seizures but a history of previous seizures while awake, the risk of further seizures while awake is higher. Therefore, a longer period of sleep-only seizures is required before driving by this group than in those who have never had a seizure while awake. This applies only to private vehicle drivers.
Seizure in a person whose epilepsy has been previously ‘well controlled’
Where a single seizure occurs after a long period (defined in these standards as at least 12 months) without seizures, the risk of further seizures is sufficiently low that driving can be resumed after a shorter period than when the epilepsy has not been as well controlled. The duration of the non-driving seizure-free period depends on whether a provoking factor was identified and can be reliably avoided (refer below). This applies only to private vehicle drivers who are already under treatment.
In people with epilepsy, their seizures are often provoked by factors such as missed doses of antiseizure medication, over-the-counter medications, alcohol or acute illnesses. If the provoking factor is avoided, the risk of subsequent seizures may be sufficiently low to allow private driving to resume after a shorter seizure-free period than following an unprovoked seizure. However, this applies only if the epilepsy has been well controlled until the provoked seizure (refer to previous point). Some provocative factors (e.g. sleep deprivation), unless severe, cannot be reliably avoided.
For the purpose of these standards, sleep deprivation is not considered a provoking factor. Refer also to Medication noncompliance .
Exceptional cases
Where a medical specialist who is experienced in managing epilepsy considers that a person with seizures or epilepsy does not meet the standards for a conditional licence but nonetheless may be safe to drive, a conditional licence may be considered if the driver licensing authority, after considering clinical information provided by the treating medical specialist, considers that the risk of a crash caused by a seizure is acceptably low.
Other factors that may influence licensing status
Several other factors may influence the management of epilepsy in regard to driving and licensing. These include:
- epilepsy treated by surgery
- medication noncompliance
- uncertain or unreliable history
- cessation of antiseizure medication
- a seizure causing a crash
- resumption of an unconditional licence.
These issues are discussed below and criteria are outlined in the table.
Epilepsy treated by surgery
Resection of epileptogenic brain tissue may eliminate seizures completely, allowing safe driving after a suitable seizure-free period. The vision standard may also apply if there is a residual visual field defect. If medication is withdrawn, refer to Withdrawal or dose reduction of one or more antiseizure medications opposite.
Medication noncompliance
Compliance with medical advice regarding medication intake is a requirement for conditional licensing. Where the treating doctor suspects noncompliance, they may recommend to the driver licensing authority that the licence be granted on the condition that periodic drug-level monitoring is conducted. Where a person without a history of noncompliance with medication experiences a seizure because of a missed dose and there were no seizures in the 12 months leading up to that seizure, the situation can be considered a provoked seizure (refer to the standard for Seizure in a person whose epilepsy has been previously well controlled above).
Uncertain or unreliable history
Some people with epilepsy are unable to reliably report the occurrence of seizures because their awareness is impaired by their seizure. Some others deliberately fail to report seizures. In both situations, the person may report that no seizures have occurred, when, in fact, they have, and the person is unfit to drive. Corroboration by people in regular contact with the person may decrease any uncertainty.
Where uncertainty remains, the driver licensing authority can be informed (refer to Part A section 3.3.1. Confidentiality, privacy and reporting to the driver licensing authority).
Withdrawal or dose reduction of one or more antiseizure medications
In people who have had no seizures while taking antiseizure medication over a suitable period, the specialist may attempt a withdrawal of all antiseizure medication, a reduction in the number of medications or a reduction in dose. The medication may also be changed because of side effects or potential side effects (e.g. teratogenicity). The person should not drive for the full period of withdrawal or dose change and for three months thereafter. However, if the dose is being reduced only because of current dose-related side effects and is unlikely to result in a seizure, driving may continue. The person will already be on a conditional licence, therefore notifying the driver licensing authority is not required. Patients who do not adhere to the prescribed dose should be reminded that compliance is a condition of their licence.
For commercial vehicle drivers, if antiseizure medication is to be withdrawn, the person will no longer meet the criteria to hold a conditional licence. This also applies to a reduction in dose of antiseizure medication except if the dose reduction is due only to the presence of dose- related side effects (refer to standards table). Driving may continue despite withdrawal of antiseizure medication only after consideration by the driver licensing authority under the Exceptional cases standard (e.g. where antiepileptic therapy has been started in a patient without seizures).
Seizure causing a crash or loss of control of a vehicle
Not all seizures carry the same risk of causing a crash or lack of control of a vehicle. People who have lost control of a vehicle as a result of a seizure are likely to have a higher crash risk. If a person who has lost control of a vehicle or experienced a crash due to a seizure, the default seizure-free non-driving period applies, even if they fall into one of the categories that allow a reduction.
Psychogenic nonepileptic seizures
Some transient episodes of impaired consciousness, awareness, or motor control resemble epileptic seizures or syncope, yet have a psychological cause. These episodes are usually termed psychogenic nonepileptic seizures (PNES), although they are sometimes known as dissociative, functional or pseudoseizures. Refer to section 7.2.9. Psychogenic nonepileptic seizures.
Resumption of an unconditional licence
Where a person has had no seizures for at least five years and has taken no antiseizure medication for at least the preceding 12 months, the driver licensing authority may consider granting an unconditional licence. This does not apply to commercial vehicle drivers.
The resumption of an unconditional private or commercial licence may be considered in some instances of first seizure or acute symptomatic seizures – refer to these entries in the table).
Medical standards for licensing – seizures and epilepsy
Requirements for unconditional and conditional licences are outlined in the following table.
Step 1: Read ‘All cases’. This applies to all people with seizures.
Step 2: Look through the list of situations in the left-hand column of the Possible reductions in the non-driving seizure-free periods for a conditional licence table to see if the person matches one of these situations.
Step 3. Look through the left-hand column of the Other factors that may influence licence status table to see if the person matches one of these situations.
Depending on the situation, the driver licensing authority may consider a conditional licence after a shorter (reduced) seizure-free period.
Note
People are not eligible for a reduction if they have had a motor vehicle crash or lost control of a vehicle due to a seizure.
If withdrawal of all antiseizure medication is planned, refer to the relevant section of the table. The longer non-driving period applies if the situation is covered by more than one standard.
All cases: default standard Health professionals should familiarise themselves with the information in this chapter and the tabulated standards before assessing a person’s fitness to drive. | ||
|---|---|---|
| Condition | Private standards (Drivers of cars, light rigid vehicles or motorcycles unless carrying public passengers or requiring a dangerous goods driver licence – refer to definition in Table 3) | Commercial standards (Drivers of heavy vehicles, public passenger vehicles or requiring a dangerous goods driver licence – refer to definition in Table 3) |
All cases (default standard) Applies to all people who have experienced a seizure. Exceptions may be considered only if the situation matches one of those listed in the tables that follow. | A person cannot hold an unconditional licence:
A conditional licence may be considered by the driver licensing authority subject to at least annual review* taking into account information provided by the treating doctor as to whether the following criteria are met:
* If a driver undergoing treatment for epilepsy has experienced an extended seizure-free period (more than 10 years) the driver licensing authority may consider reduced review requirements based on independent specialist advice (refer to section 3.3.7. Role of independent experts/panels). ** Shorter seizure-free periods may be considered by the driver licensing authority if the person’s situation matches one of those in the tables that follow. | A person cannot hold an unconditional licence:
A conditional licence may be considered by the driver licensing authority subject to at least annual review* taking into account information provided by a specialist in epilepsy as to whether the following criteria are met:
* If a driver undergoing treatment for epilepsy has experienced an extended seizure-free period (more than 20 years) the driver licensing authority may consider reduced review requirements based on independent specialist advice (refer to section 3.3.7. Role of independent experts/panels). ** Shorter seizure-free periods may be considered by the driver licensing authority if the person’s situation matches one of those in the tables that follow. *** This is only required for initial granting of the conditional licence and not for annual review. |
Possible reductions in the non-driving seizure-free periods for a conditional licence Health professionals should familiarise themselves with the information in this chapter and the tabulated standards before assessing a person’s fitness to drive. | ||
|---|---|---|
| Condition | Private standards (Drivers of cars, light rigid vehicles or motorcycles unless carrying public passengers or requiring a dangerous goods driver licence – refer to definition in Table 3) | Commercial standards (Drivers of heavy vehicles, public passenger vehicles or requiring a dangerous goods driver licence – refer to definition in Table 3) |
History of a benign seizure or epilepsy syndrome usually limited to childhood (e.g. febrile seizures, benign focal epilepsy, childhood absence epilepsy) | Private standards A history of a benign seizure or epilepsy syndrome usually limited to childhood does not disqualify the person from holding an unconditional licence, as long as there have been no seizures after 11 years of age. If a seizure has occurred after 11 years of age, the default standard (refer above) applies unless the situation matches one of those listed below. | Commercial standards A history of a benign seizure or epilepsy syndrome usually limited to childhood does not disqualify the person from holding an unconditional licence, as long as there have been no seizures after 11 years of age. If a seizure has occurred after 11 years of age, the default standard (refer above) applies unless the situation matches one of those listed below. |
First seizure (of any type) The person must report their condition to the driver licensing authority. Note: Two or more seizures in a 24-period are considered a single seizure. | Private standards A conditional licence may be considered by the driver licensing authority subject to at least annual review, taking into account information provided by the treating doctor as to whether the following criterion is met:
Resumption of an unconditional licence may be considered by the driver licensing authority, taking into account information provided by the treating doctor as to whether the following criteria are met:
| Commercial standards A conditional licence may be considered by the driver licensing authority subject to at least annual review, taking into account information provided by a specialist in epilepsy as to whether the following criteria are met:
Resumption of an unconditional licence may be considered by the driver licensing authority, taking into account information provided by a specialist in epilepsy as to whether the following criteria are met:
* This is only required for initial granting of the conditional licence and not for annual review. |
Epilepsy treated for the first time This applies when antiepileptic treatment has been started for the first time within the preceding 18 months. | Private standards A conditional licence may be considered by the driver licensing authority subject to at least annual review, taking into account information provided by the treating doctor as to whether the following criteria are met:
| Commercial standards There is no reduction. The default standard applies. |
Acute symptomatic seizures Seizures occurring only during a temporary brain disorder or metabolic disturbance in a person without previous seizures. This includes head injuries and withdrawal from drugs or alcohol. This is not the same as provoked seizures in a person with epilepsy. | Private standards A conditional licence may be considered by the driver licensing authority subject to at least annual review, taking into account information provided by the treating doctor as to whether the following criterion is met:
If there have been two or more separate transient disorders causing acute symptomatic seizures, the default standard applies. Resumption of an unconditional licence may be considered by the driver licensing authority, taking into account information provided by the treating doctor as to whether the following criteria are met:
| Commercial standards A conditional licence may be considered by the driver licensing authority subject to at least annual review, taking into account information provided by a specialist in epilepsy as to whether the following criteria are met:
If there have been two or more separate transient disorders causing acute symptomatic seizures, the default standard applies. Resumption of an unconditional licence may be considered by the driver licensing authority, taking into account information provided by a specialist in epilepsy as to whether the following criteria are met:
* This is only required for initial granting of the conditional licence and not for annual review. |
‘Safe’ seizures These are defined as seizures that do not impair driving ability (see text above). Normal responsiveness must have been tested by reliable witnesses or during video EEG. Isolated infrequent myoclonic jerks (without impaired awareness) may be considered safe in the context of no seizures of any other type for more than 12 months. | Private standards A conditional licence may be considered by the driver licensing authority subject to at least annual review, taking into account information provided by the treating doctor as to whether the following criteria are met:
If the above criteria are not met, the default standard applies. | Commercial standards There is no reduction. The default standard applies. |
Sleep-only seizures (seizures occurring only during sleep) | Private standards A conditional licence may be considered by the driver licensing authority, despite continuing seizures only during sleep and subject to at least annual review, taking into account information provided by the treating doctor as to whether the following criteria are met:
or
If the above criteria are not met, the default standard applies. | Commercial standards There is no reduction. The default standard applies. |
Seizures in a person under treatment whose epilepsy was previously well controlled ‘Well controlled’ is defined as: there were no seizures during the 12 months leading up to the last seizure. | Private standards A conditional licence may be considered by the driver licensing authority subject to at least annual review, taking into account information provided by the treating doctor as to whether the following criteria are met:
or
If the person has experienced one or more seizures during the 12 months leading up to the last seizure, there is no reduction and the default standard applies. * Sleep deprivation is not considered a provoking factor for the purpose of the standards. | Commercial standards There is no reduction. The default standard applies. |
| Exceptional cases | Private standards Where a medical specialist experienced in managing epilepsy considers that a person with seizures or epilepsy does not meet the standards above for a conditional licence but may be safe to drive, a conditional licence may be considered by the driver licensing authority, subject to at least annual review:
| Commercial standards Where a specialist in epilepsy considers that a person with seizures or epilepsy does not meet the standards above for a conditional licence but may be safe to drive, a conditional licence may be considered by the driver licensing authority, subject to at least annual review:
|
Other factors that may influence licence status Health professionals should familiarise themselves with the information in this chapter and the tabulated standards before assessing a person’s fitness to drive. | ||
|---|---|---|
| Condition | Private standards (Drivers of cars, light rigid vehicles or motorcycles unless carrying public passengers or requiring a dangerous goods driver licence – refer to definition in Table 3) | Commercial standards (Drivers of heavy vehicles, public passenger vehicles or requiring a dangerous goods driver licence – refer to definition in Table 3) |
Epilepsy treated by surgery (where the primary goal of surgery is the elimination of epilepsy) | Private standards A conditional licence may be considered by the driver licensing authority subject to at least annual review, taking into account information provided by the treating doctor as to whether the following criterion is met:
The vision standard may also apply if there is a visual field defect. If medication is withdrawn, refer to Planned withdrawal of all antiseizure medication below. | Commercial standards A conditional licence may be considered by the driver licensing authority subject to at least annual review, taking into account information provided by a specialist in epilepsy as to whether the following criteria are met:
10 years; and
The vision standard may also apply if there is a visual field defect. If any antiseizure medication is to be withdrawn, the person will no longer meet the criteria to hold a conditional licence. * This is only required for initial granting of the conditional licence and not for annual review. |
| Refusal of medical advice or medication noncompliance | Private standards Refer to the text on Refusal of medical advice and Medication noncompliance. | Commercial standards Refer to the text on Refusal of medical advice and Medication noncompliance. |
| Unreliable or doubtful clinical information | Private standards If the treating doctor doubts the reliability of the relevant clinical information (e.g. unreported seizures, likely due to the person not recognising the occurrence of seizures or deliberately not reporting seizures), the person is not fit to drive. Refer to Uncertain or unreliable history. | Commercial standards If the specialist in epilepsy doubts the reliability of the relevant clinical information (e.g. unreported seizures, likely due to the person not recognising the occurrence of seizures or deliberately not reporting seizures), the person is not fit to drive. Refer to Uncertain or unreliable history. |
| Planned withdrawal of antiseizure medication in a person who satisfies the standard to hold a conditional licence | Private standards The person should not drive:
If seizures recur, the driver licensing authority may allow the person to resume driving on a conditional licence subject to at least annual review, taking into account information provided by the treating doctor as to whether the following criteria are met:
If seizures do not recur, the person may become eligible for an unconditional licence (refer to Resumption of unconditional licence below). * If a drug is being withdrawn as part of a switch from one drug to another (e.g. to reduce teratogenic risk), the 3-month non- driving period still applies. | Commercial standards If antiseizure medication is to be withdrawn, the person will no longer meet the criteria to hold a conditional licence. Driving may continue only after consideration by the driver licensing authority under the Exceptional cases standard. |
| Recommended reduction in dosage of antiseizure medication in a person who satisfies the standard to hold a conditional licence | Private standards Driving may continue:
In circumstances other than above, the person should not drive:
If seizures recur, the driver licensing authority may allow the person to resume driving on a conditional licence subject to at least annual review, taking into account information provided by the treating doctor as to whether the following criteria are met:
| Commercial standards Driving may continue:
In circumstances other than the above, the person will no longer meet the criteria to hold a conditional licence. |
| Seizure causing a crash | Private standards If a person has experienced a crash or has lost control of the vehicle as a result of a seizure, the default seizure-free non- driving period applies, even if they fall into one of the seizure categories that allow a reduction. | Commercial standards If a person has experienced a crash or has lost control of the vehicle as a result of a seizure, the default seizure-free non- driving period applies, even if they fall into one of the seizure categories that allow a reduction. |
| Psychogenic nonepileptic seizures | Private standards | Commercial standards |
| Resumption of unconditional licence | Private standards Unless outlined in the possible reductions above (see first seizure or acute symptomatic seizure), the driver licensing authority may consider granting an unconditional licence, taking into account information provided by the treating doctor as to whether the following criteria are met:
| Commercial standards Unless outlined in the possible reductions above (see first seizure or acute symptomatic seizure), resumption of an unconditional commercial licence will not be considered. Refer to the text Resumption of unconditional licence. |
IMPORTANT: The medical standards and management guidelines contained in this chapter should be read in conjunction with the general information contained in Part A of this publication. Practitioners should give consideration to the following:
Licensing responsibility
The responsibility for issuing, renewing, suspending or cancelling a person’s driver licence (including a conditional licence) lies ultimately with the driver licensing authority. Licensing decisions are based on a full consideration of relevant factors relating to health and driving performance.
Conditional licences
For a conditional licence to be issued, the health professional must provide to the driver licensing authority details of the medical criteria not met, evidence of the medical criteria met, as well as the proposed conditions and monitoring requirements. The presence of other medical conditions While a person may meet individual disease criteria, concurrent medical conditions may combine to affect fitness to drive – for example, hearing, visual or cognitive impairment (refer to Part A section 2.2.7. Older drivers and age-related changes and section 2.2.8. Multiple medical conditions).
The nature of the driving task
The driver licensing authority will take into consideration the nature of the driving task as well as the medical condition, particularly when granting a conditional licence. For example, the licence status of a farmer requiring a commercial vehicle licence for the occasional use of a heavy vehicle may be quite different from that of an interstate multiple combination vehicle driver. The examining health professional should bear this in mind when examining a person and when providing advice to the driver licensing authority.
Reporting responsibilities
Patients should be made aware of the effects of their condition on driving and should be advised of their legal obligation to notify the driver licensing authority where driving is likely to be affected. The health professional may themselves advise the driver licensing authority as the situation requires (refer to section 3.3 and step 6).
References and further reading
- Fisher, R. S. et al. Epilepsy and driving: an international perspective. Epilepsia 35, 675–684 (1994).
- Second European Working Group on Epilepsy and Driving. Epilepsy and driving in Europe. (2005).
- Chen, W. C. et al. Epilepsy and driving: potential impact of transient impaired consciousness. Epilepsy and Behavior 30, 50–57 (2014).
- Charlton, J.L., Di Stefano, M., Dow, J., Rapoport, M.J., O’Neill, D., Odell, M., Darzins, P., & Koppel, S. Influence of chronic Illness on crash involvement of motor vehicle drivers: 3rd edition. Monash University Accident Research Centre Reports 353. Melbourne, Australia: Monash University Accident Research Centre. (2022)
- Xu, Y. et al. Prevalence of driving and traffic accidents among people with seizures: a systematic review. Neuroepidemiology 53, 1–12 (2019).
- Hansotia, P. & Broste, S. K. The effect of epilepsy or diabetes mellitus on the risk of automobile accidents. New England Journal of Medicine 324, 22–26 (1991).
- Xu, Y. et al. Who is driving and who is prone to have traffic accidents? A systematic review and meta-analysis among people with seizures. Epilepsy and Behavior 94, 252–257 (2019).
- Engel, J., Fisher, R. S., Krauss, G. L., Krumholz, A. & Quigg, M. S. Expert panel recommendations: seizure disorders and commercial motor vehicle driver safety medical expert panel members. (2007).
- Nirkko, A. C. et al. Virtual car accidents of epilepsy patients, interictal epileptic activity, and medication. Epilepsia 57, 832–840 (2016).
- Cohen, E. et al. Realistic driving simulation during generalized epileptiform discharges to identify electroencephalographic features related to motor vehicle safety: feasibility and pilot study. Epilepsia 61, 19–28 (2020).
- Lawn, N., Chan, J., Lee, J. & Dunne, J. Is the first seizure epilepsy? And when? Epilepsia 56, 1425–1431 (2015).
- Brown, J. W. L., Lawn, N. D., Lee, J. & Dunne, J. W. When is it safe to return to driving following first-ever seizure? Journal of Neurology, Neurosurgery and Psychiatry 86, 60–64 (2015).
- Krumholz, A. et al. Evidence-based guideline: management of an unprovoked first seizure in adults. Neurology 84, 1705–1713 (2015).
- Brodie, M. J., Perucca, E., Ryvlin, P., Ben- Menachem, E. & Meencke, H. J. Comparison of levetiracetam and controlled-release carbamazepine in newly diagnosed epilepsy. Neurology 68, 402–408 (2007).
- Marson, A. et al. Immediate versus deferred antiepileptic drug treatment for early epilepsy and single seizures: a randomised controlled trial. Lancet 365, 2007–2013 (2005).
- Leung, H., Man, C. B. L., Hui, A. C. F., Kwan, P. & Wong, K. S. Prognosticating acute symptomatic seizures using two different seizure outcomes. Epilepsia 51, 1570–1579 (2010).
- Beghi, E. et al. Recommendation for a definition of acute symptomatic seizure. Epilepsia 51, 671–675 (2010).
- Asadi-Pooya, A. A. et al. Driving a motor vehicle and psychogenic nonepileptic seizures: ILAE Report by the Task Force on Psychogenic Nonepileptic Seizures. Epilepsia Open 5, 371–385 (2020).
